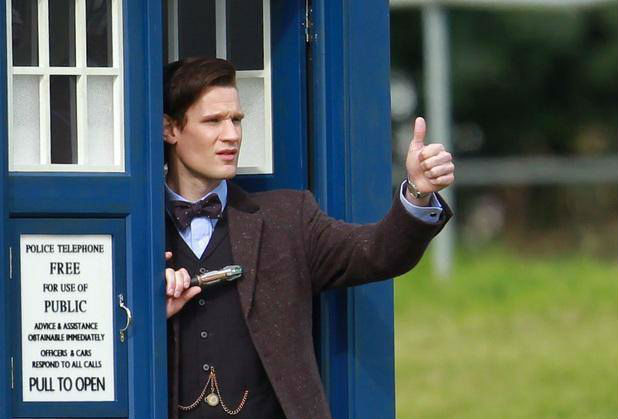
How I currently feel in specialised modality departments.
Stardate: 92458.79
I realise it's been a while since I posted anything, but I've been ridiculously busy, so I decided to wait until my first block of second year placement as a student radiographer had begun before making anything worthwhile reading... that and I've been using precious hours as nap time...
The first set of lectures were just a bombardment of anatomy, and believe me when I say we learn a good deal more than just bones! Thankfully, it's my strong subject, but alongside Anatomy is Imaging Science (or Physics), Imaging Technique and Research Methods (queue the 'Psycho' theme). I've suddenly realised that my home away from home is the Healthcare Library, and copious note-making (seriously, it's ridiculous how tall my pile of notes is) accompanied by rivers of green tea is helpful. And as that wasn't challenging me enough, attending four martial arts classes a week while being captain of the university Taekwondo club certainly assured I learned to appreciate weekends in a whole new light. I've forgotten what sleep is.... again.
This year, I'm in a completely different Trust for placement, so aside from getting used to new radiographers, specialised modality departments (such as CT), different shift times and learning which direction I'm supposed to be going in, I've also had to brush off the cobwebs cluttering my radiographically-trained brain in order to not look completely useless!
For my first week, I was placed in Vascular, which involves angiography, an imaging technique that visualises the blood vessels using contrast agents. You also get to live in scrubs for a week. One of the examinations I saw this week was a cerebral angiogram (within the brain's vessels), that displayed 6 aneurysms in the patient's brain. These were treated with endovascular coiling, which involves inserting a guided catheter (small wire) into the femoral artery (in the thigh/groin area), which aids a microcatheter into the aneurysm. This coiling promotes blood clotting within the aneurysm, eventually sealing it and reducing the pressure.
But my favourite experience this week, happened to be during an endarterectomy, which is the surgical removal of plaque from an artery. This examination can be quite slow for radiographers, as they are only needed for a small part of the procedure. Luckily, my supervisor knew the surgeon taking the case, asked if I could observe the procedure. The surgeon agreed and basically explained everything to me as if I were his student.
Throughout this procedure, patients stay awake but are anaesthetised. An incision is then made over the blockage site (in this case the femoral artery), and the blood flow is re-routed using clamps. The artery is then opened, and the plaque removed. As student radiographers don't go into dissection rooms, I was amazed to see how big the femoral artery is in 'real life'; about the thickness of your little finger. It was brilliant to be able to understand what was actually going on, instead of just aiding the radiologist, who inserted a shunt further up the artery, to 're-inflate' the artery, to prevent the artery staying narrowed.
Overall, this week was really interesting, although I've been told many students find Vascular placement quite boring. I think it is what you make of it, and I did my best to get involved as much as possible, for example changing contrast, patient moving and handling etc. It's also a good time to learn some vascular anatomy, such as the various branches of the internal carotid artery. You also get to see a 3D spin, which is a pretty cool radiograph of the skull that does almost a 360 view, with contrast to help visualise the cerebral vessels. Check out this Youtube link for an example: http://www.youtube.com/watch?v=0gWmehOhRGs
Next week I'm in Main X-Ray again, so I'll get to refresh what I learnt from first year (and maybe get a head-start on my portfolio). Hopefully I'm not too rusty!
LLAP guys!